The Gastroparesis Food Sequencing Method: Optimizing Meal Composition and Texture for Improved Emptying
Introduction
Gastroparesis, also known as delayed gastric emptying, is a chronic gastrointestinal condition that impairs the stomach’s ability to efficiently move food to the small intestine. This condition affects millions globally, particularly individuals with diabetes, certain neurological disorders, and idiopathic causes where no definitive origin is identified. Symptoms such as early satiety, bloating, nausea, vomiting, and malnutrition can make daily life challenging.
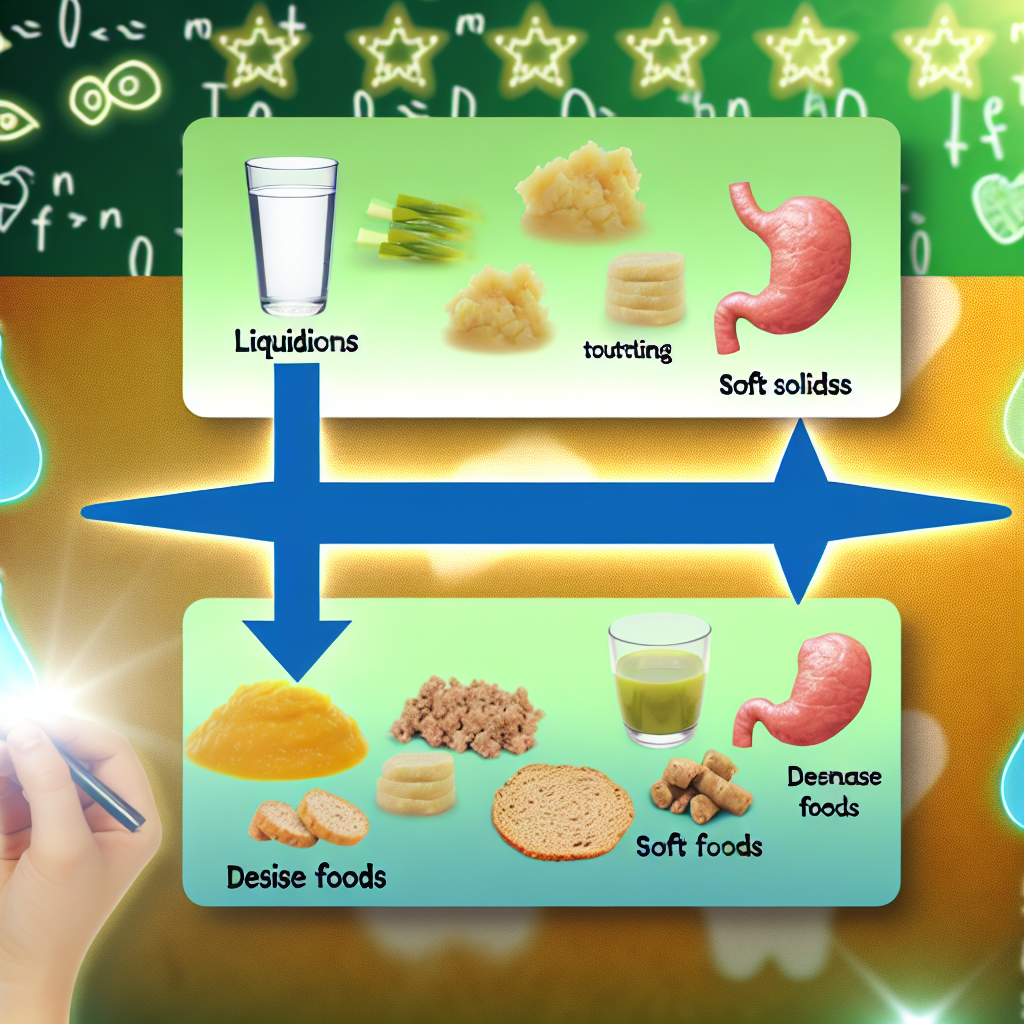
Emerging strategies rooted in functional nutrition offer promising alternatives to manage gastroparesis symptoms with fewer side effects than medications or surgery. One such innovation is the Gastroparesis Food Sequencing Method: a structured approach to meal planning where foods are consumed in a systematic order—starting with liquids and progressing to soft and then denser solids—to promote more effective gastric emptying.
Traditional gastroparesis diets focus on reducing fat and fiber and promoting small, frequent meals. Food sequencing adds a new dimension by factoring in food timing and texture. By consuming easily digestible, hydrating foods first, the digestive system is primed to handle more complex textures, aiding motility and nutrient absorption.
This method also resonates with ancient traditions like Ayurveda and Traditional Chinese Medicine, which emphasize mindful eating and strategic food ordering. Together with modern science, this holistic approach offers renewed hope for natural gastroparesis management.
This article explores the foundational principles of food sequencing, clinical evidence supporting its efficacy, practical tips for implementation, and guidelines on optimizing the composition and texture of meals to enhance gastrointestinal function.
Features: Medical and Professional Studies Supporting Food Sequencing for Gastroparesis
Medical literature increasingly acknowledges the potential benefits of food sequencing for gastroparesis. Though novel in Western diets, its physiological foundation is strong—and research is growing.
A pivotal pilot study from the journal Neurogastroenterology and Motility (2018) investigated how sequence impacts postprandial blood sugar and gastric emptying in diabetic individuals. The study found that consuming protein and healthy fats before carbohydrates led to more stable blood glucose and smoother digestion. For gastroparesis patients struggling with blood sugar fluctuations and delayed emptying, this sequencing strategy can be transformative.
The American Journal of Gastroenterology published clinical guidelines recommending low-residue, low-fat, and low-fiber meals. Researchers noted that starting a meal with hydrating, pureed foods enhances gastric neuromuscular activity, preparing the stomach for more complex foods. This sequencing improved symptoms such as bloating and minimized the formation of bezoars (indigestible food masses).
Texture matters too. A 2020 guideline from the Society for Surgery of the Alimentary Tract emphasized eating pureed or blended meals to aid in gastric propulsion. Sequencing from liquid to soft to semi-solid maintains a consistent, digestible meal structure that supports improved motility.
Research by the University of Michigan Health System shows that combining food sequencing with prokinetic drugs and herbal remedies like ginger and Iberogast enhances symptom control. Patients using a combination of these therapies experienced measurable improvements in early satiation, bloating, and abdominal discomfort.
Despite the small-scale nature of current studies, the evidence steadily supports using food sequencing to manage symptoms naturally. Advocates highlight its capacity to enhance digestive coordination and reduce reliance on medication.
Practical Implementation: How to Use Food Sequencing
To incorporate food sequencing for gastroparesis, follow a structured eating flow:
– Begin with clear fluids or broths to hydrate, stimulate gastric nerves, and ease into mealtime.
– Follow with pureed or blended foods like smoothies, vegetable soups, or applesauce.
– Then gradually introduce soft solids such as mashed potatoes, yogurt, or scrambled eggs.
– Conclude the meal with denser, chewed foods, avoiding tough meats or fibrous vegetables when symptoms are severe.
Meals should remain small and frequent—typically 5–6 meals per day. Chew thoroughly, avoid carbonated drinks, and sit upright during and after meals to facilitate gravitational gastric emptying.
Special care should be taken for those with severe symptoms. In those cases, a nutritionist or gastroenterologist can tailor sequencing for individual tolerance and symptom profiles.
Conclusion
The Gastroparesis Food Sequencing Method offers a strategic, holistic way to improve digestive outcomes for people living with delayed gastric emptying. By reordering food consumption, adjusting textures, and emphasizing nutrient timing, this method aligns both with modern science and time-tested traditions. It enhances gastric motility, minimizes discomfort, and reduces complications—an empowering, low-risk approach for symptom management.
As a complementary method alongside medications, herbal aids, or lifestyle changes, food sequencing serves as a flexible and individualized aid. Its thoughtful design makes it an approachable, non-invasive solution for millions navigating gastroparesis.
Concise Summary
The Gastroparesis Food Sequencing Method is a holistic approach to managing delayed gastric emptying by strategically ordering the consumption of foods—from fluids to purees to solids—to enhance gastric motility and reduce symptoms. Supported by clinical research and traditional medicine practices, this method helps alleviate nausea, bloating, and early fullness while optimizing nutrient absorption. Implementing structured meals, focusing on texture and composition, and integrating herbs and medications can make food sequencing a powerful, personalized strategy for improving digestion and quality of life in gastroparesis patients.
References
5. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Gastroparesis.”

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com