Understanding Ulcerative Colitis and Its Impact
Ulcerative colitis inflammatory bowel disease is a chronic condition that presents a significant challenge to patients and healthcare providers alike. Characterized by inflammation and ulceration of the colon and rectum, UC can cause symptoms such as abdominal pain, diarrhea, fatigue, and rectal bleeding. The condition often follows a relapsing-remitting course, making long-term management crucial.
Evolution of Treatment Options
Over the past decade, medical advancements have transformed the treatment landscape for UC. While traditional therapies like corticosteroids and 5-aminosalicylic acid remain foundational, newer options, including biologics and small-molecule drugs, have significantly enhanced the ability to control inflammation and improve patients’ quality of life. These innovations target specific inflammatory pathways, providing more tailored and effective approaches to treatment.
Current Therapeutic Landscape
This article delves into the current therapeutic options for UC, emphasizing recent advances in biologics, immunomodulators, and innovative treatments. By understanding these options, patients and clinicians can make informed decisions about managing the disease and achieving remission.
5-ASA Medications: Primary Treatment Approach
These medications reduce inflammation by inhibiting the production of inflammatory mediators in the colon. 5-ASA drugs for mild to moderate UC, such as mesalamine, are often the first line of treatment.
Role of Corticosteroids in Treatment
Prednisone and other corticosteroids are effective for acute flare-ups, rapidly reducing inflammation. Long-term use is discouraged due to significant side effects including osteoporosis, weight gain, and increased infection risk.
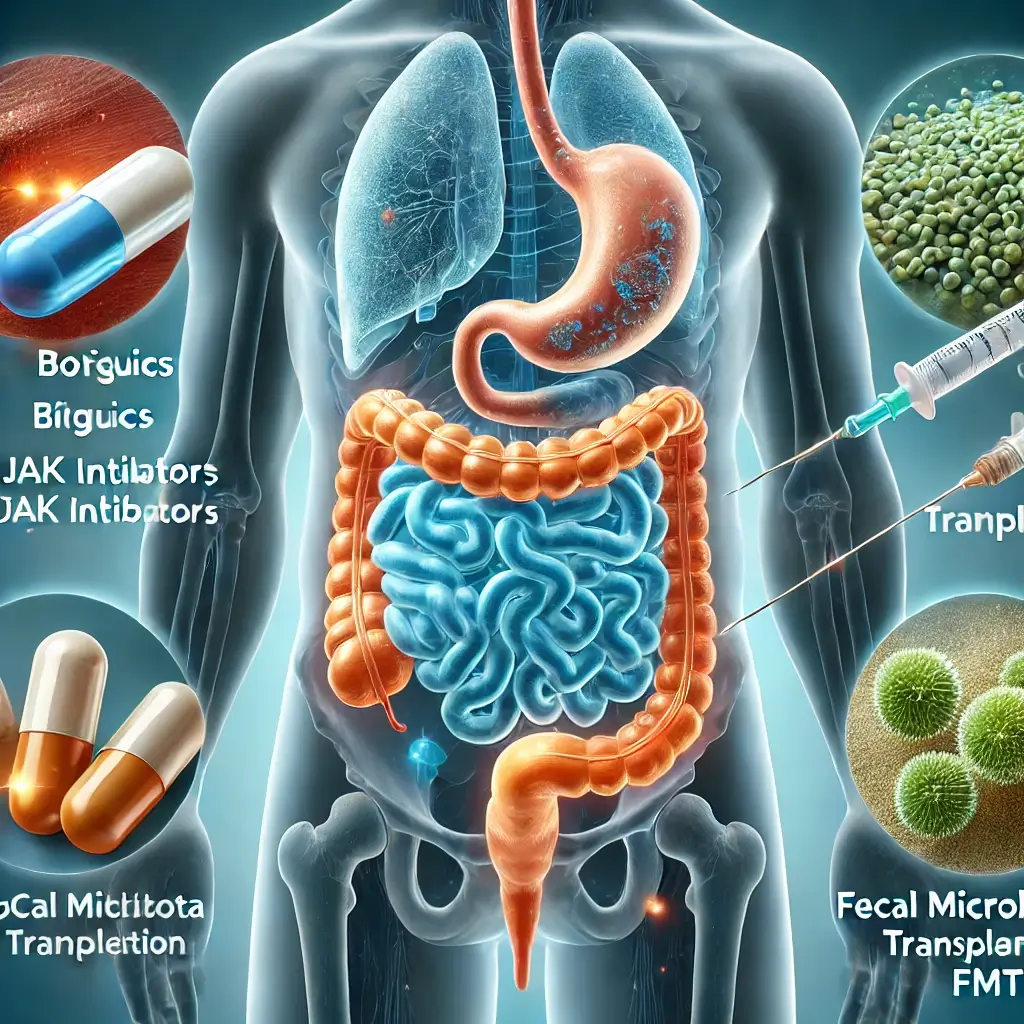
Biologic Therapy Advancements
Biologics are protein-based drugs derived from living organisms. They target specific components of the immune system involved in inflammation. TNF-α inhibitors like infliximab and adalimumab block TNF-α, a cytokine central to UC’s inflammatory process. Integrin inhibitors such as vedolizumab target molecules that mediate immune cell migration to the gut. Newer biologics, like ustekinumab, inhibit interleukin-12 and interleukin-23.
JAK Inhibitors: Oral Treatment Innovation
Small-molecule drugs like tofacitinib represent a class of oral medications that block Janus kinase pathways, crucial for cytokine signaling. These inhibitors offer a convenient oral alternative to injectable biologics.
Emerging Microbiota-Based Treatments
Fecal microbiota transplantation for ulcerative colitis treatment involves transplanting stool from a healthy donor to restore a balanced gut microbiome. Research indicates promising results, with some studies reporting remission rates exceeding 40% in refractory cases.
Stem Cell Therapy Potential
Mesenchymal stem cell infusions for tissue repair is under investigation for its potential to repair damaged tissue and modulate the immune response. Early-phase trials suggest safety and efficacy, but more research is needed.
Treatment Personalization and Challenges
Not all patients respond uniformly to biologics or JAK inhibitors. Pharmacogenomics and biomarkers for predicting treatment response are increasingly used to tailor therapies. Advanced therapies can be prohibitively expensive, limiting access for many patients.
Future of UC Management
The advent of biologics, JAK inhibitors, and other advanced therapies has revolutionized the treatment landscape. These innovations have significantly improved the ability to achieve and sustain remission. However, challenges such as cost, accessibility, and individualized treatment response underscore the need for continued research and development.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com