Bile Acid Malabsorption: The Overlooked Cause of Chronic Diarrhea
Introduction
Chronic diarrhea is a frustrating and often debilitating condition that affects many people worldwide. While conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and infections are commonly investigated as causes, one lesser-known yet significant reason for persistent diarrhea is Bile Acid Malabsorption (BAM).
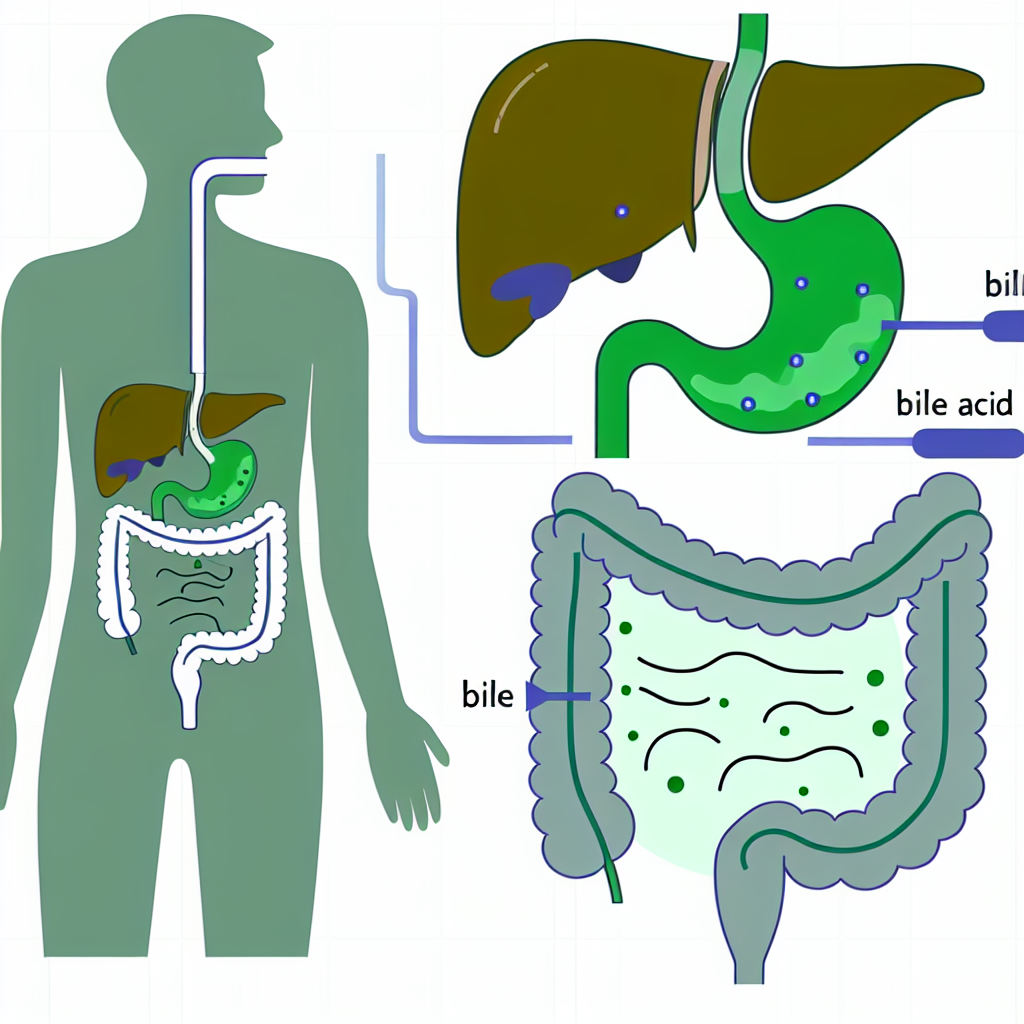
Bile acids play a crucial role in digestion, particularly in the breakdown and absorption of dietary fats. Normally, these acids are produced in the liver, stored in the gallbladder, and released into the small intestine after eating. Once bile acids have aided digestion, around 95% of them are reabsorbed in the ileum (the last part of the small intestine) and recirculated through the liver to be reused. However, when this process is disrupted, excess bile acids spill into the colon, leading to irritation, watery diarrhea, urgency, bloating, and abdominal discomfort.
BAM is often categorized into three types:
1. Type 1 BAM – Caused by diseases affecting the ileum, such as Crohn’s disease, surgical removal of the ileum, or radiation therapy.
2. Type 2 BAM (Primary BAM) – A condition where BAM occurs without any apparent underlying gastrointestinal disease.
3. Type 3 BAM – Associated with other conditions like IBS, small intestinal bacterial overgrowth (SIBO), and pancreatic disorders.
Many healthcare providers overlook BAM, often misdiagnosing it as IBS-D (Irritable Bowel Syndrome with Diarrhea). According to research, up to 30-50% of individuals diagnosed with IBS-D may actually have BAM. Despite its impact on quality of life, BAM remains underdiagnosed due to a lack of awareness and difficulty in accessing diagnostic tests such as the SeHCAT scan (used primarily in Europe).
Understanding BAM is the first step toward addressing chronic diarrhea effectively. The good news is that natural and herbal treatments can help support gut health, improve bile acid regulation, and reduce symptoms. In this article, we’ll explore medical insights and natural approaches to improving bile acid reabsorption and overall digestive function.
What Does Research Say About Bile Acid Malabsorption?
Multiple scientific studies highlight the impact of BAM and its role in chronic diarrhea. A 2015 study published in the journal *Gut* found that BAM is a frequent but often misdiagnosed cause of functional diarrhea and IBS-D patients, reinforcing the importance of proper diagnosis ([Camilleri, 2015](https://pubmed.ncbi.nlm.nih.gov/25187440/)).
Another key research piece from *Alimentary Pharmacology & Therapeutics* indicated that up to 50% of patients with IBS-D may have underlying BAM, reinforcing the necessity for proper testing and management of bile acid levels ([Slattery et al., 2022](https://pubmed.ncbi.nlm.nih.gov/34831912/)).
Additionally, gallbladder removal (cholecystectomy) has been associated with a higher risk of BAM due to continuous bile acid release into the intestines instead of regulated secretion ([Shariati et al., 2018](https://pubmed.ncbi.nlm.nih.gov/29197992/)). This leads to irritation of the colon, frequent loose stools, and increased urgency.
How Is BAM Diagnosed?
Testing for BAM is still not widespread, but notable diagnostic methods include:
– SeHCAT test: A specialized nuclear medicine scan that measures bile acid retention.
– Fecal Bile Acid Test: Analyzes bile acid levels in stool samples.
– Serum C4 Test: Measures a bile acid precursor in the blood to assess synthesis rates.
Conventional Treatment for BAM
Physicians often prescribe bile acid sequestrants such as cholestyramine (Questran), colestipol, or colesevelam to manage BAM. While these medications can be effective, they may cause side effects such as constipation, bloating, and interference with fat-soluble vitamin absorption. This makes natural alternatives an attractive option for many individuals dealing with BAM.
Top Natural Remedies for Bile Acid Malabsorption
If you suspect BAM or have been diagnosed with the condition, incorporating natural therapies and gut-friendly habits can make a significant difference in symptoms and overall digestive health. Below are key natural approaches to managing BAM effectively:
1. Psyllium Husk – A Natural Bile Acid Binder
Psyllium is a natural fiber that helps bind excess bile acids in the intestines and regulate bowel movements. A study published in the *Journal of Neurogastroenterology and Motility* found that psyllium supplementation improved stool consistency and frequency in individuals with functional diarrhea ([Eswaran et al., 2017](https://pubmed.ncbi.nlm.nih.gov/27647618/)).
2. Soothing Herbs: Slippery Elm and Marshmallow Root
These herbs possess soothing and mucilaginous properties, which help coat the intestinal lining and reduce irritation caused by bile acids. They protect the gut from inflammation, reducing diarrhea and urgency.
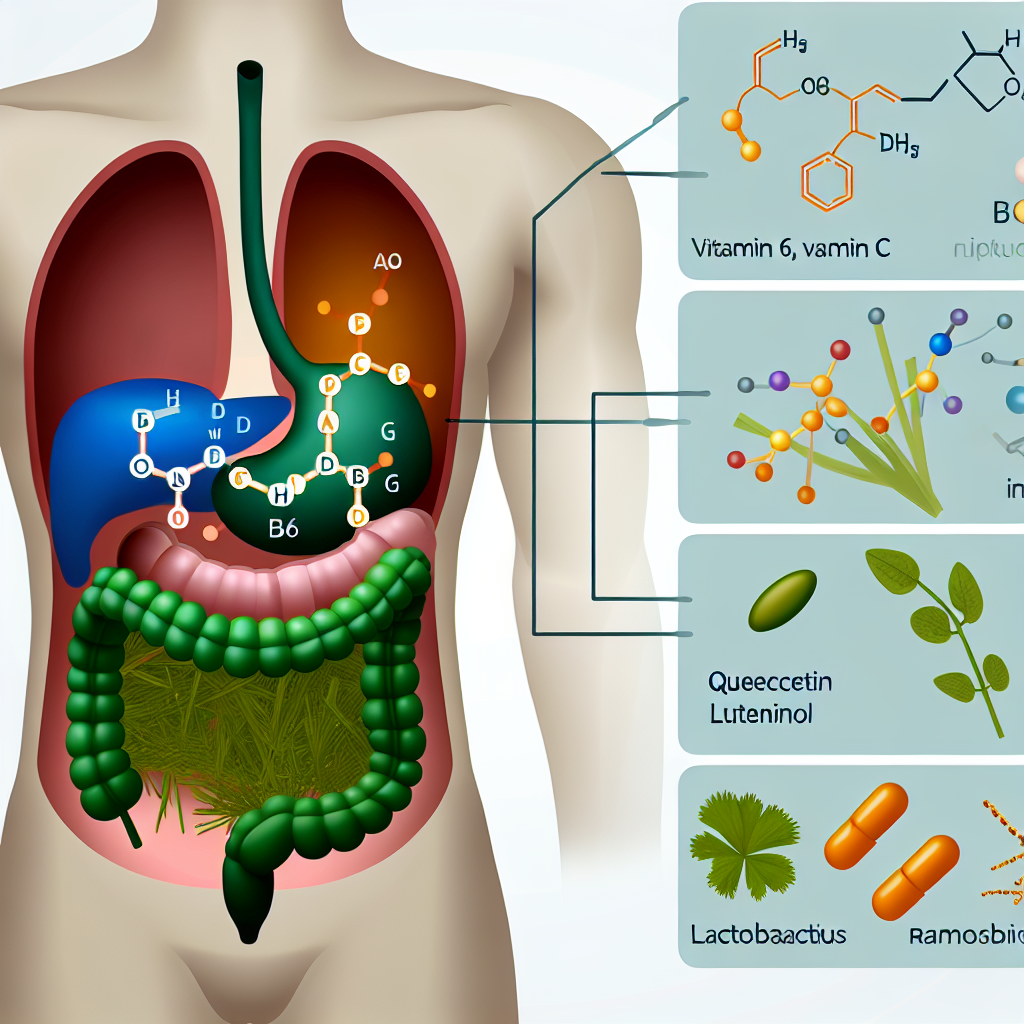
3. Probiotics – Balancing Gut Bacteria
Lactobacillus and Bifidobacterium strains have been shown to improve bacterial balance in the gut and aid in bile acid metabolism. A 2021 study in *Frontiers in Microbiology* found that probiotics help regulate excess bile acid by promoting gut microbiome diversity, which is crucial for gut health ([Markowiak-Kopeć & Śliżewska, 2021](https://www.frontiersin.org/articles/10.3389/fmicb.2021.642723/full)).
4. Aloe Vera and Chamomile – Nature’s Digestive Healers
Aloe vera helps maintain gastrointestinal balance and reduces inflammation. Chamomile acts as a natural antispasmodic and can calm IBS-D-related digestive discomfort.
5. Green Banana and Pectin-Rich Foods
Green bananas contain resistant starch, which helps bind excess bile acids and reduce diarrhea. Apples (with the skin) and citrus fruits are rich in pectin, a natural prebiotic fiber that strengthens the gut lining.
6. Turmeric & Curcumin – Reducing Inflammation Naturally
Turmeric, a natural anti-inflammatory powerhouse, helps reduce gut irritation caused by bile acids. A review from *Phytotherapy Research* cited curcumin’s effectiveness in reducing symptoms of digestive disorders, including diarrhea and gut permeability issues ([Hewlings & Kalman, 2017](https://pubmed.ncbi.nlm.nih.gov/28994385/)).
7. Low-Fat and Anti-Inflammatory Diet
Since bile acids are primarily used in fat digestion, consuming excessive fats can exacerbate symptoms. A diet high in lean proteins, non-starchy vegetables, and fiber-rich foods supports digestive health while minimizing excess bile acid excretion. Reducing fried and processed foods, dairy, and excessive caffeine can further prevent irritation and recurrent diarrhea.
8. Dandelion Root & Milk Thistle – Supporting Liver Function
Both of these herbs support liver function and bile acid metabolism, promoting proper reabsorption. They may be beneficial in individuals with compromised liver function who experience bile acid dysregulation.
Conclusion: Take Control of Your Gut Health
Bile Acid Malabsorption is an often overlooked but significant cause of chronic diarrhea affecting many individuals. While it is commonly misdiagnosed as IBS-D, proper testing and natural interventions can significantly improve symptoms and overall gut function. Scientific studies confirm the importance of identifying BAM early and managing it with a combination of dietary modifications, herbal treatments, and gut-friendly habits.
Leveraging natural remedies such as psyllium husk, probiotics, anti-inflammatory herbs, and fiber-rich foods can help bind excess bile acids, regulate intestinal function, and promote long-term gut health. If you struggle with chronic diarrhea and suspect BAM, consult a healthcare provider for appropriate testing and consider integrating these natural therapies into your daily routine for optimal digestive well-being.
**Summary:**
Bile Acid Malabsorption (BAM) is a common but often overlooked cause of chronic diarrhea. It occurs when bile acids, which are crucial for fat digestion, are not properly reabsorbed in the small intestine. This leads to excess bile acids spilling into the colon, causing irritation, watery diarrhea, and other digestive issues. Natural remedies like psyllium husk, probiotics, soothing herbs, and anti-inflammatory foods can help manage BAM and improve overall gut health. Consulting a healthcare provider for proper testing and incorporating these natural approaches can significantly alleviate symptoms and promote long-term digestive well-being.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com