Crohn’s Disease: Natural Support Methods for Symptom Relief
Introduction
Crohn’s disease is a chronic inflammatory condition that affects the gastrointestinal (GI) tract, most commonly the small intestine and colon. As an autoimmune disorder, Crohn’s disease occurs when the immune system mistakenly attacks the digestive tract lining, leading to symptoms such as abdominal pain, severe diarrhea, fatigue, weight loss, and malnutrition. While conventional treatments such as immunosuppressive drugs, corticosteroids, and biologics can help manage symptoms, many patients seek natural and holistic methods to complement traditional care.
Natural remedies and lifestyle interventions can play a crucial role in managing symptoms, reducing inflammation, and improving overall gut health. Certain herbal treatments, probiotics, anti-inflammatory diets, and stress management techniques have shown promise in alleviating discomfort and promoting remission in patients with Crohn’s disease.
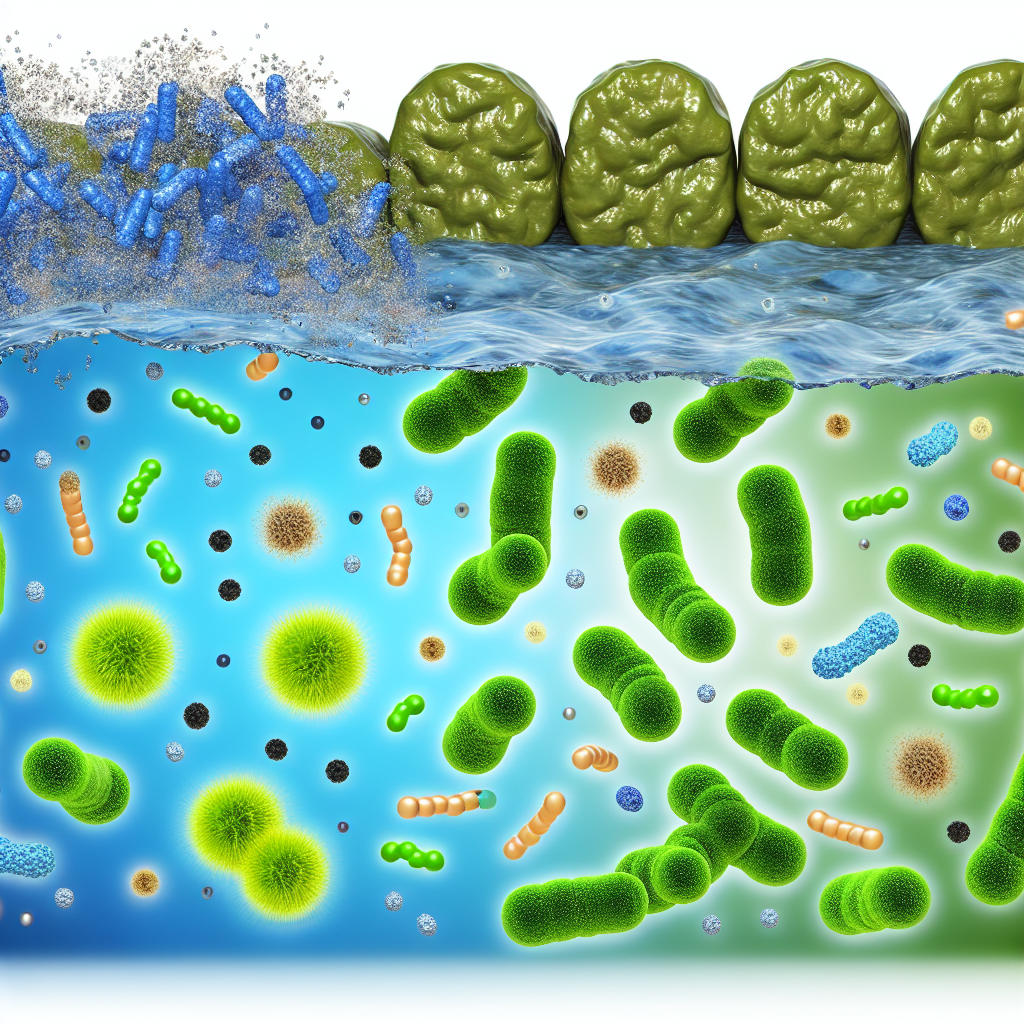
Understanding the relationship between gut health and the immune system is essential for exploring viable natural interventions. The gut microbiome, which consists of trillions of beneficial bacteria, plays a fundamental role in digestion, immune function, and inflammation. Research has shown that disruptions in gut microbiota (dysbiosis) may contribute to Crohn’s disease flare-ups and heightened immune responses. Therefore, strategies that support microbiome balance and reduce gut inflammation are particularly beneficial.
The Power of Diet: Managing Crohn’s Disease Through Nutrition
Research indicates that an anti-inflammatory diet can significantly reduce symptoms in Crohn’s disease patients. Studies suggest that specific dietary approaches, such as the Mediterranean diet, may lower disease activity by reducing inflammation (Singh et al., 2017). A diet rich in omega-3 fatty acids, found in wild-caught fish, flaxseeds, and walnuts, has been shown to decrease inflammatory markers associated with Crohn’s disease.
Moreover, eliminating common dietary triggers—such as processed foods, refined sugars, and dairy—can prevent symptom exacerbation. The Specific Carbohydrate Diet (SCD) and Low-FODMAP diet have demonstrated effectiveness in managing Crohn’s symptoms by reducing gut inflammation and restoring microbiome balance (Suskind et al., 2018).
Probiotics and Prebiotics: Restoring Gut Microbiome Balance
Since an imbalance in gut bacteria is a common factor in Crohn’s disease, probiotics and prebiotics may help regulate symptoms. A meta-analysis published in *Frontiers in Medicine* suggests that probiotic strains such as *Lactobacillus* and *Bifidobacterium* can promote gut healing and improve microbiota composition (Shen et al., 2014).
Prebiotic foods—such as chicory root, garlic, and asparagus—support beneficial bacterial growth, which is vital for maintaining gut health. Incorporating both probiotics and prebiotics into the diet may help fortify the gut microbiome, potentially reducing the severity of Crohn’s disease symptoms.
Herbal Remedies: Natural Anti-Inflammatory Support
Several herbs have shown promise in Crohn’s disease symptom management:
– Turmeric (Curcumin): A 2020 study in *Nutrients* highlighted curcumin’s ability to reduce inflammation by inhibiting inflammatory cytokines in Crohn’s patients (Ghosh et al., 2020).
– Aloe Vera: Known for its soothing effects on the digestive tract, aloe vera has demonstrated potential in reducing gastrointestinal inflammation.
– Licorice Root: Glycyrrhizin, a compound found in licorice root, has been studied for its anti-inflammatory and mucosal protective effects in inflammatory bowel diseases (Rahmani et al., 2015).
These herbs can be consumed as teas, supplements, or in their natural form to help ease Crohn’s-related inflammation and support gut healing.
Stress Management: The Key to Reducing Flare-Ups
Chronic stress has been linked to increased inflammation and exacerbation of Crohn’s symptoms. A study published in *Clinical Gastroenterology and Hepatology* found that stress management techniques, including mindfulness meditation and yoga, improved quality of life and reduced flare-ups in Crohn’s patients (Mawdsley & Rampton, 2005).
Practicing deep breathing exercises, progressive muscle relaxation, and acupuncture can help regulate the immune response and decrease disease severity. By incorporating these methods into daily life, individuals can better manage emotional and physical stressors that contribute to Crohn’s disease flare-ups.
Conclusion
While Crohn’s disease is a lifelong condition with no definitive cure, natural support methods can significantly improve symptom management and overall gut health. Dietary interventions, probiotics, herbal remedies, and stress-reducing practices offer promising complementary strategies for enhancing digestive function and reducing inflammation. As scientific research continues to uncover insights into the gut microbiome and immune regulation, integrating holistic therapies into a comprehensive treatment plan can provide meaningful relief for those struggling with Crohn’s disease.
Individuals should always consult their healthcare provider before making any significant lifestyle changes or incorporating supplements to ensure safety and effectiveness in their treatment regimen.
Summary:
Crohn’s disease is a chronic inflammatory condition affecting the gastrointestinal tract. While conventional treatments can help manage symptoms, natural remedies and lifestyle interventions, such as anti-inflammatory diets, probiotics, herbal remedies, and stress management techniques, can play a crucial role in alleviating discomfort and promoting remission. By integrating these holistic approaches, individuals with Crohn’s disease can take empowered steps toward better digestive health and long-term remission.
References:
[Read More](https://www.mdpi.com/2072-6643/12/3/715)
[Read More](https://www.cghjournal.org/article/S1542-3565(05)00127-6/fulltext)
[Read More](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4462051/)
[Read More](https://pubmed.ncbi.nlm.nih.gov/24445604/)
[Read More](https://pubmed.ncbi.nlm.nih.gov/27548731/)
[Read More](https://pubmed.ncbi.nlm.nih.gov/29976438/)

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com