Oxalate Management for Gut Health: A Dietary and Supplemental Strategy for Sensitive Individuals
Introduction
Gut health has garnered growing attention in recent years, as modern research increasingly connects digestive wellness to immune resilience, nutrient absorption, and even brain function. Among the many factors impacting the digestive system, oxalates—naturally occurring compounds in certain plant-based foods—have emerged as a potential disruptor for individuals with sensitive gastrointestinal systems.
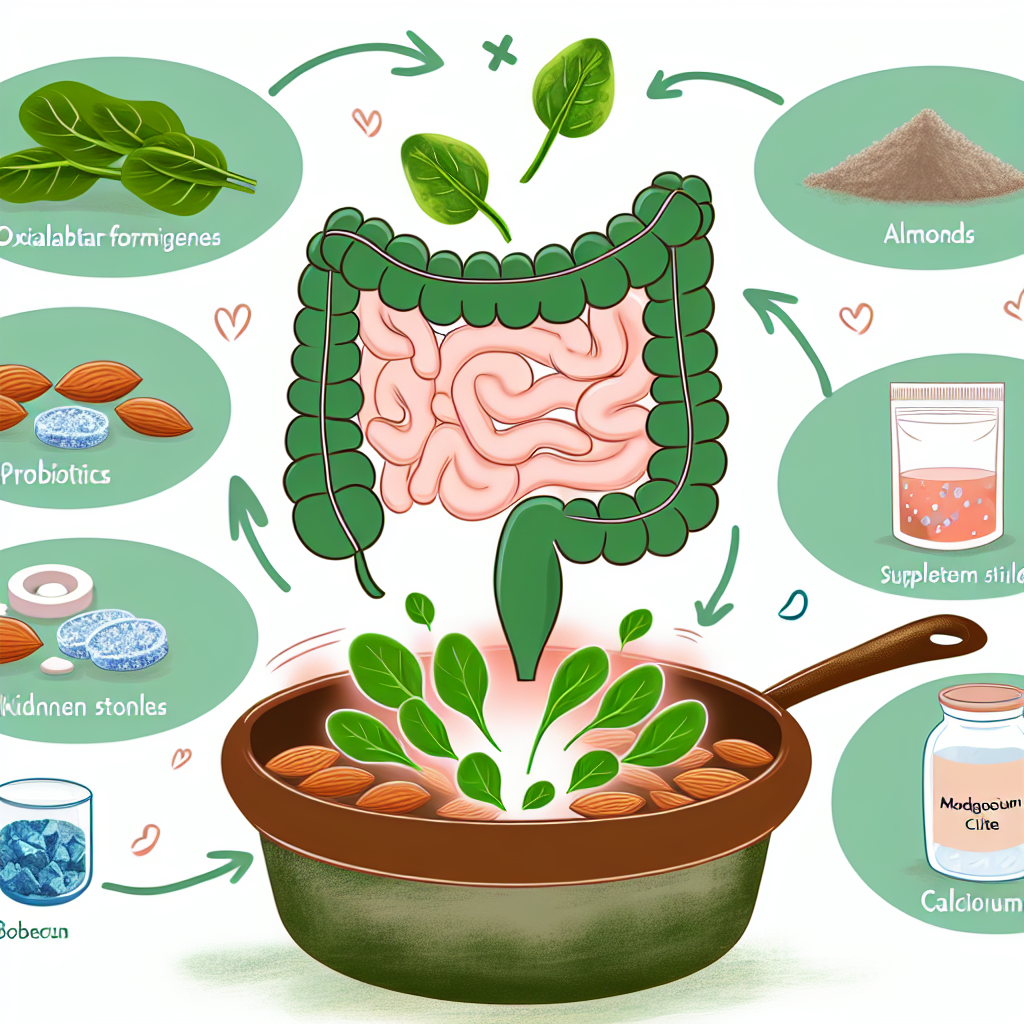
Oxalates, or oxalic acid derivatives, are prevalent in a wide range of nutritious foods, including spinach, beets, rhubarb, sweet potatoes, almonds, cashews, and dark chocolate. In a healthy digestive system, these compounds are typically broken down by oxalate-degrading bacteria and excreted safely in urine. However, for some individuals—especially those with existing gut conditions, kidney dysfunction, or microbial imbalances—oxalates can build up, contributing to issues such as kidney stones, joint inflammation, chronic fatigue, and even neurological discomfort.
One of the key players in oxalate metabolism is the gut microbiome. Research has shown that microbial diversity, particularly the presence of bacteria such as Oxalobacter formigenes, plays a vital role in preventing pathological oxalate accumulation. Unfortunately, this bacterium is easily diminished by antibiotics, poor diet, gut inflammation, or stress, leaving susceptible individuals more prone to oxalate-related symptoms.
This presents a unique challenge: How can people sensitive to oxalates maintain a nutrient-rich diet—often full of fresh vegetables, nuts, and legumes—without exacerbating their symptoms? Eliminating all high-oxalate foods isn’t sustainable or nutritious, and many of these foods offer extensive health benefits beyond their oxalate content.
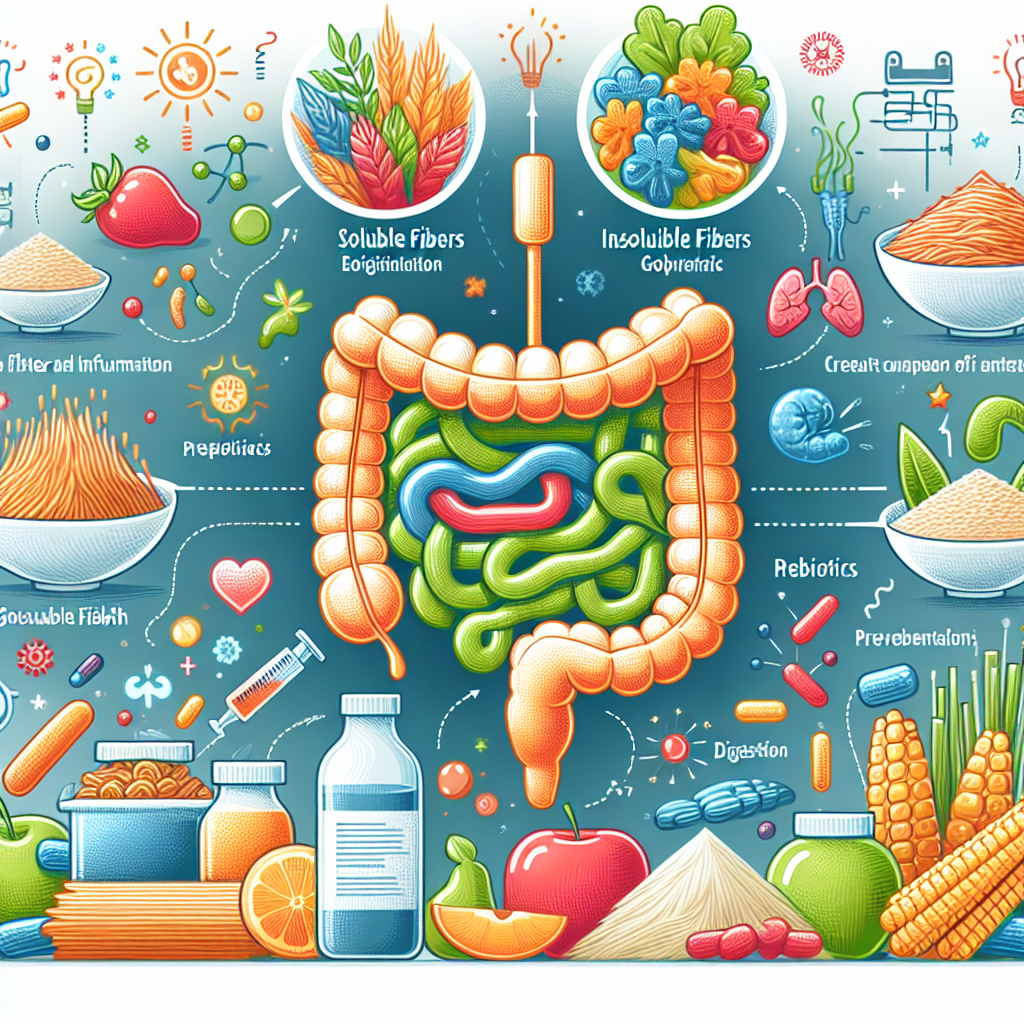
A more sustainable solution lies in an integrative strategy. This includes dietary moderation of oxalates, cooking techniques to reduce oxalate content (like boiling or soaking), restoring microbial balance through probiotics, and using specific supplements such as calcium and magnesium to bind and neutralize oxalates internally.
This guide delves deeper into how oxalates influence gut health, offers tools for identifying and managing high-oxalate foods, explores the scientific evidence behind microbial and supplement-based interventions, and outlines a natural path toward personalized oxalate management. The result is a clearer, more empowered approach to gut health that supports vitality and long-term resilience.
Medical & Professional Studies on Oxalate and Gut Health
A growing body of scientific research underscores the deep connection between the gut microbiome and oxalate metabolism. Disruptions in this system can lead to a cascade of issues, including oxalate buildup, kidney stones, and systemic inflammation.
One pivotal study published in the Journal of the American Society of Nephrology explored the impact of a specific oxalate-degrading bacterium, Oxalobacter formigenes. Researchers found that individuals lacking this bacterium were significantly more likely to develop hyperoxaluria—a condition that causes excess oxalates in urine—and were at higher risk for developing calcium oxalate kidney stones (Siener et al., 2013). The takeaway: maintaining a robust microbiome is critical for efficient oxalate clearance.
Further research, published in Kidney International, showed that antibiotic exposure can drastically reduce or eliminate O. formigenes from the colon. In the absence of this bacteria, oxalate absorption increases, heightening the risk for oxalate-related complications (Kaufman et al., 2010). This highlights the importance of either preventing antibiotic overuse or pursuing probiotic therapy post-treatment to restore microbial health.
Speaking of probiotics, a clinical trial out of the University of Chicago tested Lactobacillus and Bifidobacterium strains in adults following a low-oxalate diet. After incorporating these strains for several weeks, participants showed reduced urinary oxalate excretion. This finding, published in Clin Ther (Campieri et al., 2006), suggests that even in the absence of O. formigenes, other beneficial microbes may assist in breaking down dietary oxalates.
From a nutritional standpoint, a significant review in Asia Pacific Journal of Clinical Nutrition emphasized the importance of cooking preparation over complete food elimination. Techniques like soaking beans or boiling spinach can slash oxalate levels by up to 80% (Noonan & Savage, 1999), allowing individuals to enjoy more nutrient-dense foods without overwhelming their system.
Supplement-wise, calcium citrate and magnesium citrate have demonstrated efficacy in reducing oxalate absorption. According to a clinical evaluation published in Urology Research and Practice (Atmani et al., 2003), calcium citrate taken with meals can bind dietary oxalates, forming insoluble compounds that the body safely excretes through the bowel.
These combined insights reinforce the value of an integrative oxalate strategy: one that harnesses the power of microbiome support, mindful food preparation, and targeted nutrient supplementation to create an effective, lifestyle-based pathway toward gut health and oxalate balance.
Conclusion
For individuals navigating symptoms related to gut sensitivity, inflammation, or kidney stone formation, understanding and managing dietary oxalates can lead to noticeable improvement in comfort and overall health. Rather than adopting unnecessarily restrictive diets, a holistic, evidence-backed approach empowers individuals to maintain a full spectrum of nutrients while minimizing the negative impact of oxalates.
Optimizing the gut landscape with beneficial bacteria, preparing meals to reduce oxalate load, and using therapeutic supplements like calcium and magnesium citrate create a comprehensive defense against oxalate-related disturbances. These strategies not only support oxalate metabolism but also reinforce the broader goals of reducing inflammation, enhancing digestion, and promoting nutrient assimilation.
By considering oxalates as one key variable in a larger gut health picture—and applying a strategic approach tailored to individual biochemistry and lifestyle—sensitive individuals can regain control over their health. Whether you’re healing from chronic gastrointestinal conditions or seeking to prevent future imbalances, an integrative oxalate management plan offers a sustainable path forward.
For more on gut health strategies and dietary solutions, visit www.gutnow.com.
References
1. Siener R, et al. J Am Soc Nephrol, 2013.
2. Kaufman DW, et al. Kidney Int, 2010.
3. Campieri C, et al. Clin Ther, 2006.
4. Noonan SC, Savage GP. Asia Pac J Clin Nutr, 1999.
5. Atmani F, et al. Urology Research and Practice, 2003.
Concise Summary
This guide explores the impact of dietary oxalates on gut health, especially in sensitive individuals. Oxalates, found in many plant-based foods, can exacerbate issues like kidney stones or inflammation when gut bacteria like Oxalobacter formigenes are deficient. Scientific evidence supports using methods like soaking and boiling foods, consuming probiotics, and taking calcium or magnesium supplements to mitigate oxalate absorption. A practical and sustainable approach balances oxalate reduction with nutrition, offering a personalized path toward improved digestive and overall health.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com