Understanding Common Digestive Health Issues
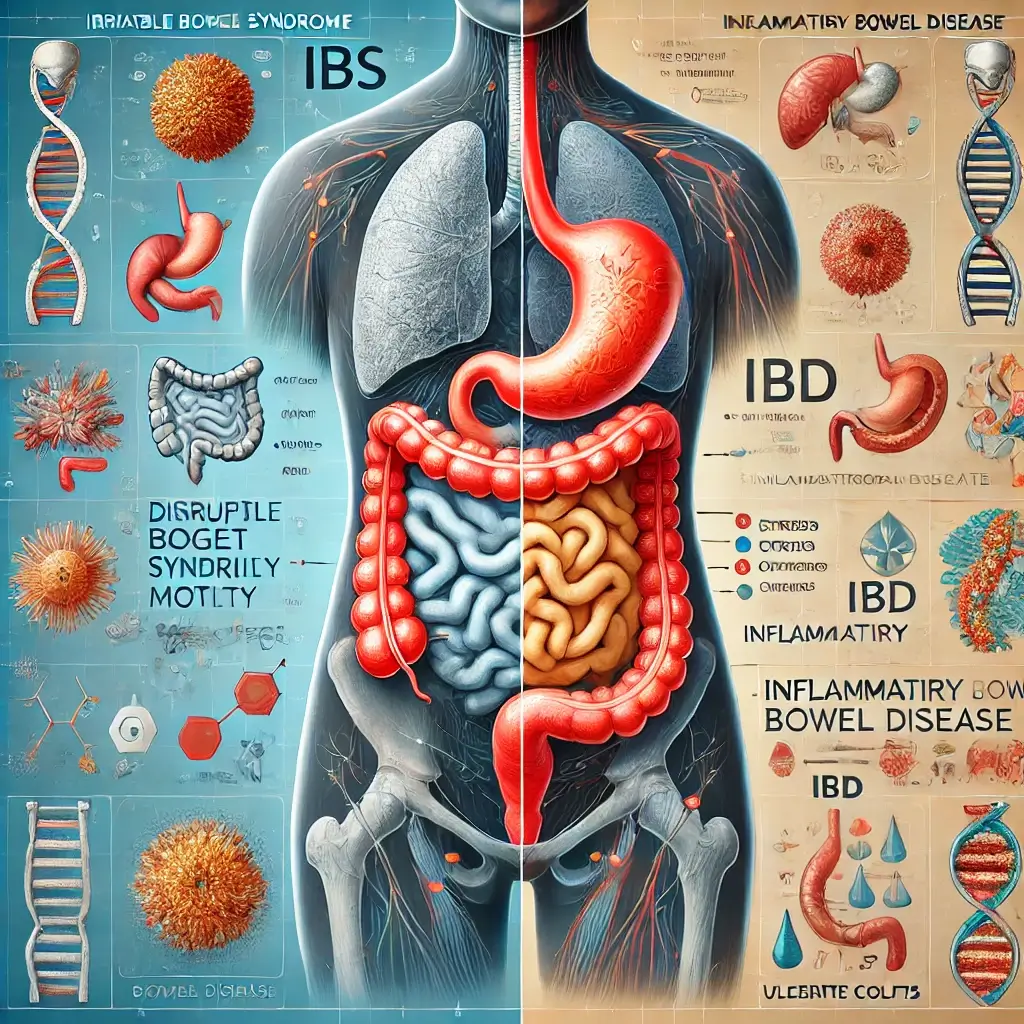
Digestive health issues are among the most common medical concerns, affecting millions worldwide. Among these, Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD) are two frequently discussed yet often misunderstood conditions. While they share overlapping symptoms like abdominal pain and altered bowel habits, they differ significantly in their causes, severity, and management strategies. This distinction is critical for proper diagnosis and treatment, and improved patient outcomes.
Critical Distinctions in Gastrointestinal Conditions
IBS is classified as a functional gastrointestinal disorder, where the gut’s function is disrupted without structural damage. In contrast, IBD is an autoimmune disease marked by chronic inflammation and damage to the digestive tract, including Crohn’s disease and ulcerative colitis. Understanding these conditions is essential for patients, caregivers, and healthcare professionals to address symptoms effectively and navigate long-term health challenges.
Introduction to Comprehensive Analysis
This article dives into the key distinctions between IBS and IBD, integrating recent research and clinical guidelines to provide a comprehensive understanding of these conditions.
Core Differences Between IBS and IBD
Exploring the Differences Between IBS and IBD
Understanding Root Causes
1. Causes and Mechanisms
Origins of IBS
IBS:
The exact cause of IBS is not fully understood. Research suggests that it may involve a combination of abnormal gut motility, visceral hypersensitivity, and disruptions in the gut-brain axis. Stress, anxiety, and certain foods often act as triggers, exacerbating symptoms. Emerging evidence also links IBS to gut microbiota imbalances and low-grade intestinal inflammation.
Understanding IBD Development
IBD:
IBD arises from an immune system malfunction, where the body mistakenly attacks the digestive tract’s lining. This leads to chronic inflammation and tissue damage, and complications such as fistulas and strictures. Genetic predisposition, environmental factors, and gut microbiome dysbiosis contribute to disease onset.
Recognizing Symptoms
2. Symptoms and Presentation
Identifying IBS Manifestations
IBS Symptoms:
IBS typically causes abdominal pain and bloating, and changes in bowel habits (diarrhea, constipation, or both). These symptoms are episodic, triggered by stress or certain foods, and often improve after a bowel movement. Unlike IBD, IBS does not cause rectal bleeding or weight loss.
Recognizing IBD Indicators
IBD Symptoms:
IBD symptoms include chronic diarrhea and rectal bleeding, abdominal pain and fatigue, and unintentional weight loss. Symptoms are often persistent and can lead to complications such as nutrient deficiencies and anemia. IBD may also manifest with extraintestinal symptoms, such as joint pain or skin conditions.
Diagnostic Methods
3. Diagnostic Approaches
IBS Diagnosis Protocol
IBS:
Diagnosing IBS involves ruling out other conditions. Physicians use criteria like the Rome IV guidelines and may conduct stool and blood tests, along with imaging, to exclude other disorders. There is no specific biomarker for IBS, making the diagnosis largely clinical.
IBD Diagnosis Process
IBD:
IBD diagnosis requires a combination of blood tests and stool tests, imaging (CT or MRI), and colonoscopy with biopsies. These tools help identify inflammation, ulcers, and structural damage. Biomarkers such as C-reactive protein and fecal calprotectin are commonly used to assess disease activity.
Treatment Strategies
4. Treatment Options
Managing IBS Effectively
IBS Management:
Since IBS has no cure, treatment focuses on symptom management. This includes dietary modifications (e.g., low-FODMAP diet), stress reduction, and medications targeting specific symptoms (e.g., antispasmodics, laxatives). Probiotics and gut-directed psychotherapies have also shown promise in managing symptoms.
Treating IBD Comprehensively
IBD Treatment:
IBD treatment aims to reduce inflammation and manage symptoms, and prevent flare-ups. This typically involves anti-inflammatory medications, immune suppressants, and biologic therapies. In severe cases, surgery may be necessary to remove damaged sections of the digestive tract.
Latest Research Developments
Recent studies emphasize the role of the gut microbiome in both IBS and IBD. In IBS, interventions such as fecal microbiota transplants and prebiotics are being explored to restore microbial balance. For IBD, advancements in biologic therapies, including anti-TNF agents and integrin inhibitors, have significantly improved outcomes for patients with severe disease.
Evolution of Dietary Approaches
Additionally, dietary therapies continue to evolve. While a low-FODMAP diet remains a cornerstone for IBS management, exclusive enteral nutrition and elimination diets are gaining traction in IBD care, particularly in children and young adults.
Final Insights
IBS and IBD, though frequently confused, represent distinct gastrointestinal conditions with unique causes, symptoms, and treatment approaches. Recognizing these differences is vital for timely and effective medical intervention. With ongoing research and advancements in treatment options, patients with IBS or IBD have more tools than ever to manage their conditions and improve their quality of life.
Seeking Professional Help
If you experience persistent digestive symptoms, consult a healthcare professional. Proper diagnosis and tailored treatment can make all the difference in managing your gut health.
Research Citations
References
Longstreth, J. F., et al. (2016). Functional Gastrointestinal Disorders: Fourth Rome Criteria. Gastroenterology, 150(6), 1392–1402. PMC.
Loftus, E. V., et al. (2017). Clinical Practice Guidelines for Inflammatory Bowel Disease in Adults. Gastroenterology, 152(6), 1471–1500. PMC.
Ford, A. C., et al. (2020). Advances in the Diagnosis and Treatment of Irritable Bowel Syndrome. Nature Reviews Gastroenterology & Hepatology, 17(8), 473–486.
Pittayanon, R., et al. (2019). Gut Microbiota in Patients With Irritable Bowel Syndrome—A Systematic Review. Gastroenterology, 157(1), 97–108.
Ni, J., et al. (2017). Gut Microbiota and IBD: Causation or Correlation? Nature Reviews Gastroenterology & Hepatology, 14(10), 573–584.
Feuerstein, J. D., et al. (2020). Systematic Review and Meta-Analysis of Anti-TNF Therapy for Inflammatory Bowel Disease. Alimentary Pharmacology & Therapeutics, 51(8), 740–751.
Mullish, B. H., et al. (2020). The Use of Faecal Microbiota Transplant as Treatment for Recurrent or Severe Clostridium difficile Infection and Other Potential Indications. Journal of Internal Medicine, 288(6), 678–694.
Sigall-Boneh, R., et al. (2017). Dietary Therapy With the Crohn’s Disease Exclusion Diet Is a Successful Strategy for Induction of Remission in Children and Young Adults Failing Biological Therapy. Journal of Crohn’s and Colitis, 11(10), 1205–1212.

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com