Elemental Diet Transition Strategy: How to Reintroduce Foods and Rebuild Flora After a Gut Reset
Introduction
For those managing chronic gut conditions like Small Intestinal Bacterial Overgrowth (SIBO), Irritable Bowel Syndrome (IBS), or inflammatory bowel disorders, the elemental diet offers a scientifically-supported tool for healing. This nutrition-only formula provides broken-down nutrients, allowing the digestive system to rest and regenerate by reducing pathogenic bacteria and gut inflammation.
However, the real challenge arises after completing the diet: transitioning back to whole foods and rebuilding the gut microbiome—both of which are critical in maintaining the healing progress. Many patients make the mistake of reintroducing regular meals too quickly, which can reignite symptoms and compromise recovery results.
Since the elemental diet “resets” the gut, it’s imperative to repopulate healthy microbes while reinforcing the gut lining. A staged and measured reintroduction of food helps reduce the risk of symptom flare-up and enables long-term digestive resilience.
Restoring gut health post-elemental diet involves both cellular nourishment and microbial recolonization. This requires a deliberate approach—guided by nutrition science, clinical biomarkers, and awareness of post-diet sensitivities. When done correctly, people often experience steady digestion, enhanced mental clarity, and improved immunity.
In this comprehensive guide, we outline an evidence-based strategy backed by current clinical research to help you successfully re-enter the world of real food after an elemental reset.
Scientific Backing for Post-Elemental Diet Recovery Strategies
Recent clinical studies have shown a clear consensus: a structured recovery following an elemental diet is crucial for sustained results. In a landmark study by Dr. Mark Pimentel and colleagues ([Pimentel et al., 2004](https://doi.org/10.1023/B:DDAS.0000037794.43155.82)), a 14–21-day elemental protocol achieved an 80% success rate in reducing symptoms like bloating and abnormal breath tests in SIBO patients. However, the relapse rate remained high unless a transition and maintenance plan was in place.
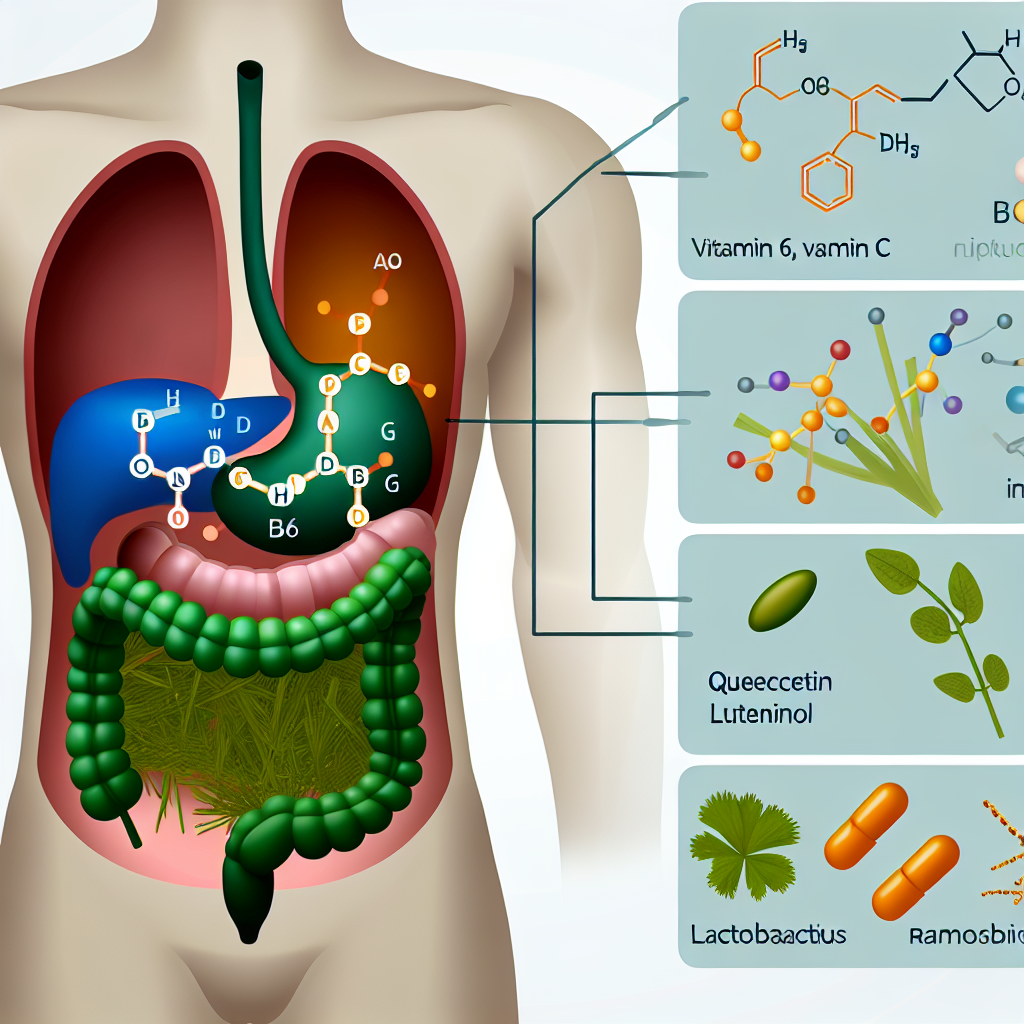
The elemental diet drastically reduces microbial diversity, including the beneficial species needed for long-term gut stability. A study published in [Cell Host & Microbe](https://doi.org/10.1016/j.chom.2018.08.002) confirms that restricted diets compromise microbial ecosystems, leaving the gut susceptible to re-infection and inflammation. Reseeding the flora using prebiotic-rich foods and targeted probiotics becomes essential to re-establish balance and resilience.
The Low-FODMAP Reintroduction Protocol, developed by [Monash University](https://www.monashfodmap.com), provides a careful path to discern individual sensitivities by gradually adding fermentable carbohydrates back into the diet.
Also, nutritional support of gastrointestinal integrity is critical. L-glutamine, a key amino acid found in elemental formulas, has been shown in studies such as one published in [Nutrients (Wang et al., 2017)](https://doi.org/10.3390/nu9090998) to promote gut lining repair by strengthening tight junctions and supporting mucosal integrity.
Botanical remedies like slippery elm, marshmallow root, and deglycyrrhizinated licorice (DGL) offer soothing benefits for the epithelial lining. Meanwhile, collagen-rich foods, bone broth, and anti-inflammatory nutrients like zinc, vitamin A, and omega-3 fatty acids provide the building blocks needed for tissue repair and immune support.
Scientific literature supports a slow transition back to whole foods, prioritizing nutrient-rich, low-reactivity ingredients to optimize gut resilience and symptom-free functioning.
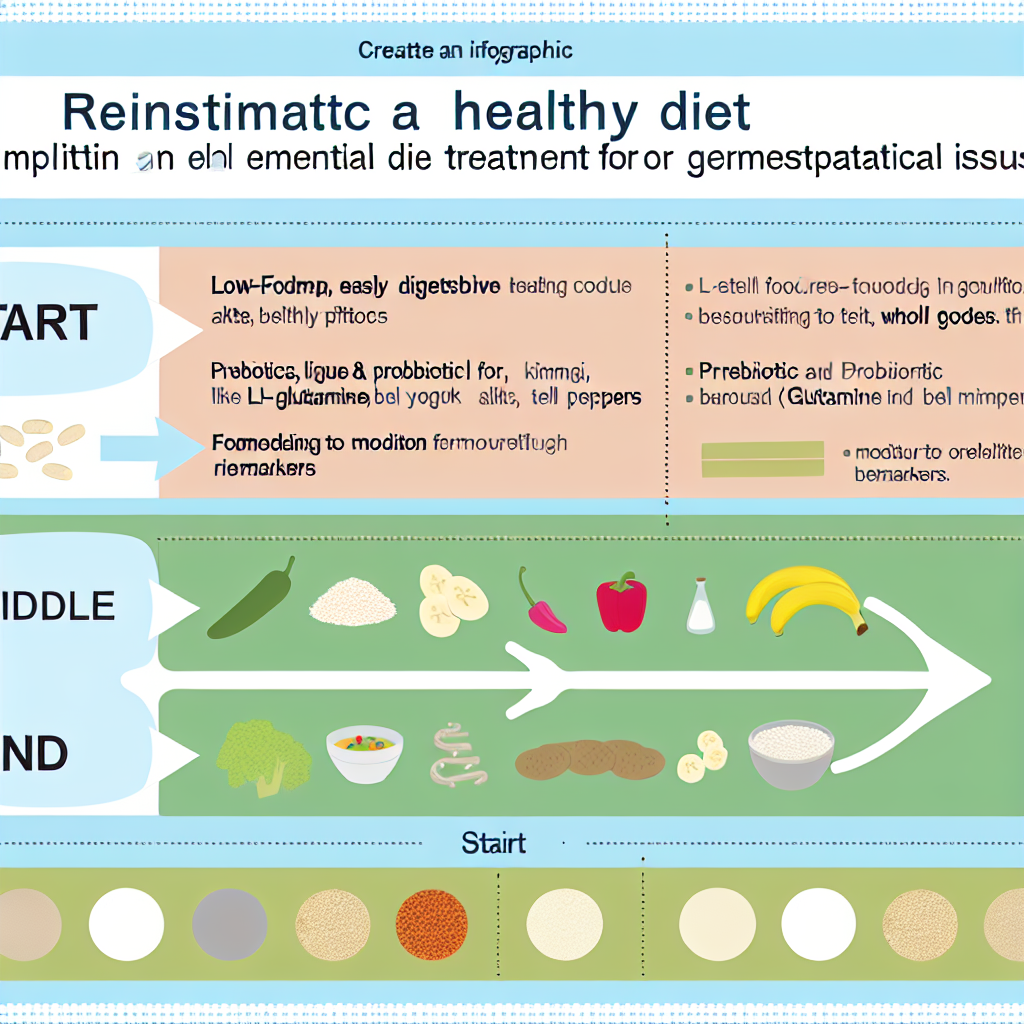
Step-by-Step Elemental Diet Transition Strategy
Week 1–2: Simple, Low-FODMAP Vegetables and Proteins
Start with the most easily digestible foods. Recommended foods include:
– Soft, low-FODMAP vegetables such as zucchini, spinach, and carrots, cooked to reduce fiber complexity.
– Light proteins such as chicken, turkey, fish, and eggs, slowly introduced in small amounts. Bone broth and poached meats are ideal starters to minimize gut workload.
– Avoid all raw vegetables, legumes, high-FODMAP fruits like apples, and grains.
– Add gut-lining support through daily supplementation of L-glutamine, slippery elm powder, or aloe vera juice.
– Hydrate consistently and introduce herbal teas like ginger or peppermint to encourage digestion without stimulating fermentation.
This phase focuses on introducing foods that are unlikely to disrupt the still-fragile microbiome or cause gas and bloating.
Week 3–4: Introduce Resistant Starches and Prebiotic Fibers
Once digestion improves, integrate low-dose fermentable foods to start rebuilding microbial diversity:
– Resistant starches including cold, cooked potatoes (retrograded starch), green bananas, cooked oats, or quinoa.
– Prebiotic-rich but low-FODMAP fruits such as kiwi and blueberries.
– Introduce small amounts of fermented foods—homemade coconut yogurt, sauerkraut, or kefir—to provide natural strains of beneficial bacteria.
– Continue supplementation with glutamine and collagen peptides to support tissue repair.
Begin food journaling to track digestive responses, ensuring tolerance before increasing portion sizes.
Week 5–6: Transition to a Gut-Healthy Lifestyle Diet
Now the gut should be ready to handle moderately complex foods.
– Introduce a greater variety of vegetables, grains, fruits, and lean proteins.
– Begin trialing small amounts of high-FODMAP foods—garlic, onions, lentils, apples—one at a time and spaced by 72 hours to isolate any trigger.
– Increase polynutrient load with foods rich in polyphenols (berries, olives, green tea), omega-3 fatty acids (wild salmon, chia seeds), and fermented foods to feed and diversify microbial populations.
– Periodically incorporate gut-rest days with light broths to prevent overburdening digestion.
Keep monitoring physical and mood symptoms to catch intolerance patterns.
Ongoing Support
Maintaining gut health over the long term includes:
– Working with a professional nutritionist or functional medicine provider to measure microbial diversity, nutrient status, and gut lining integrity using stool and serum testing (e.g., zonulin, calprotectin, microbiome analysis).
– Maintaining an anti-inflammatory diet: leafy greens, olive oil, turmeric, wild fish, fermented foods like miso and kimchi.
– Practicing mindful eating, stress reduction, and ample hydration.
– Periodic use of restorative gut practices such as bone broth fasts or intermittent fasting days to support long-term mucosal health.
– Using food rotation techniques to avoid food sensitivity development over time.
Conclusion
Successfully coming off an elemental diet requires patience, structure, and a deep understanding of gut ecology. While the elemental diet resets the microbiome and allows for gut lining repair, it is the post-diet strategy that ensures the body maintains these improvements. Through careful food reintroduction, targeted prebiotics and probiotics, and integrative support with herbs and nutrients, individuals can rebuild a resilient digestive system.
Attention to microbial diversity, symptom tracking, and proper supplementation ensures that the gut remains sealed, populated with beneficial microbes, and free from inflammatory triggers. With mindful planning, individuals can not only maintain remission but also enhance vitality, cognitive clarity, and metabolic wellbeing for the long term.
Concise Summary
The elemental diet is a powerful tool for treating gut disorders like SIBO and IBS, but transitioning off it requires careful strategy. This guide outlines a phased food reintroduction plan to prevent relapse, focusing on gut-healing foods, prebiotics, and probiotics. Weeks 1–2 emphasize low-FODMAP, simple proteins and vegetables. Weeks 3–4 introduce resistant starches to seed microbiota. By weeks 5–6, a full gut-healthy diet is adopted. Ongoing support includes lab testing, anti-inflammatory diets, and continued microbiome care. Structured recovery ensures lasting gut health and protection against future dysbiosis.
References
1. [Pimentel, M., et al. (2004). Digestive Diseases and Sciences](https://doi.org/10.1023/B:DDAS.0000037794.43155.82)
2. [Sonnenburg, E.D., and Sonnenburg, J.L. (2018). Cell Host & Microbe](https://doi.org/10.1016/j.chom.2018.08.002)
3. [Monash University – Low FODMAP Diet](https://www.monashfodmap.com)
4. [Wang, B., et al. (2017). Nutrients – L-glutamine and Tight Junctions](https://doi.org/10.3390/nu9090998)
5. [Slavin, J. (2013). Nutrients – Fiber and Prebiotics](https://doi.org/10.3390/nu5051417)

Dominic E. is a passionate filmmaker navigating the exciting intersection of art and science. By day, he delves into the complexities of the human body as a full-time medical writer, meticulously translating intricate medical concepts into accessible and engaging narratives. By night, he explores the boundless realm of cinematic storytelling, crafting narratives that evoke emotion and challenge perspectives.
Film Student and Full-time Medical Writer for ContentVendor.com